Your Pharmacy Benefits at A Glance
Before you fill a prescription, it can be helpful to review the basics about how your pharmacy coverage works.
As a new Select Health member—or even if you’ve been with us a while—you might need some help figuring out your pharmacy benefits. We can help you understand how your pharmacy coverage works.
How do I know if a medication is covered?
Log in to Select Health Member Account to find out how much a drug costs. Once you’re logged in, click the Pharmacy tab to use tools that will help you find the cost of drug and lower cost options available to you.
You can also look at your Select Health ID card—it will tell you what prescription drug list is covered by your plan. Visit our Pharmacy Benefits page and select your drug list to find the most commonly covered medications.
If you still have questions, call Member Services to speak with someone on our Pharmacy team. They can help you understand if a specific drug is covered by your plan.
Related: Get Your Medications with Hassle-free Home Delivery
How do I know what my prescription copay will be?
All medications are in a tier that is based on your plan. Each tier corresponds to a specific copay or coinsurance amount—this is the amount you pay when you fill the prescription. These tiers may include:
- Preferred generic and generic drugs – lowest cost
- Nonpreferred generic drugs
- Preferred brand name drugs – higher cost
- Nonpreferred brand name drugs – highest cost
- Specialty oral and injectable drugs
Medications that fall in to lower tiers may provide the treatment you need at the best value.
How can I find a pharmacy or compare drug prices?
Log in to your Select Health Member Account as described above, and you’ll be able to:
- Search for a participating pharmacy near you
- See what drugs are covered using your prescription drug list
- View claims for prescriptions you have already filled
What is step therapy and preauthorization?
For some medications, we require step therapy or preauthorization before they will be covered. If your medication requires step therapy, your doctor must first prescribe a more cost-effective medication (i.e., trying a generic drug before the name-brand). In some cases, step therapy and preauthorization may be waived for medical necessity.
Still have questions? Call us at 800-538-5038.
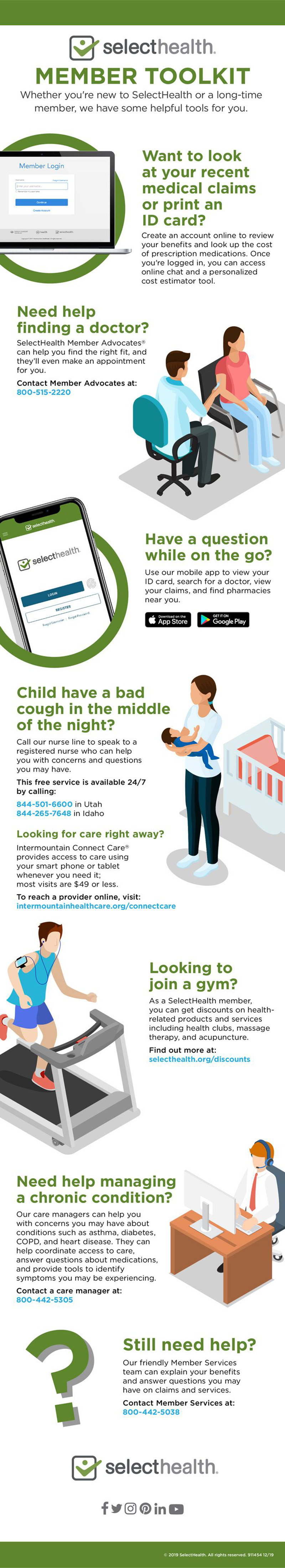
Related: Select Health Member Toolkit