Select Health Medicare
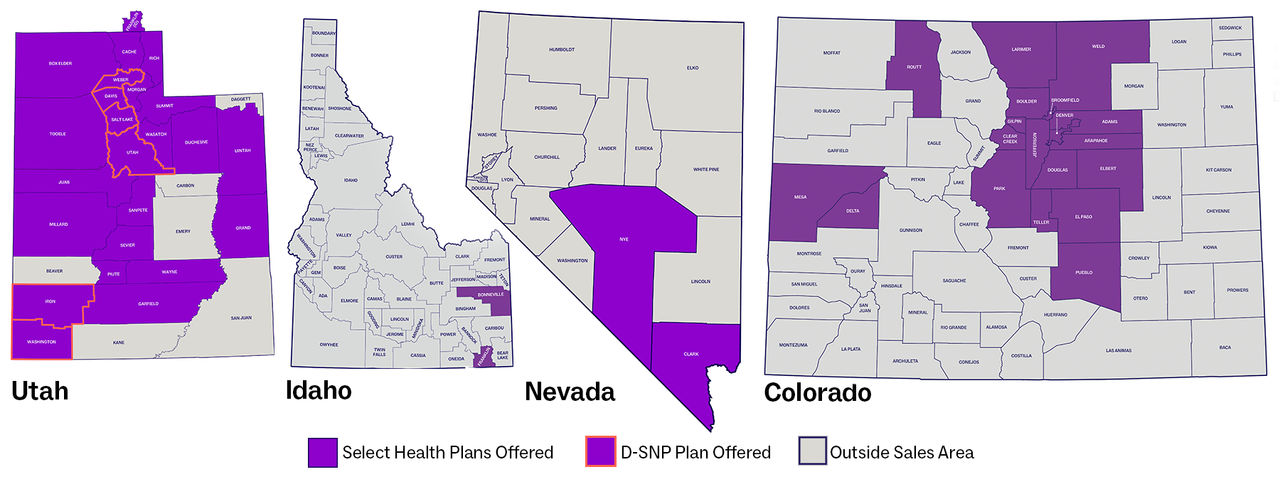
2024 Select Health Medicare plans for Medicare Advantage beneficiaries are available to residents in Utah, Idaho, Nevada, and Colorado based on the coverage maps below.
2024 Select Health Medicare plans for Medicare Advantage beneficiaries are available to residents in Utah, Idaho, Nevada, and Colorado based on the coverage maps below.
Physicians and other healthcare professionals who participate on Select Health Medicare agree to comply with the standards and regulations set forth by the Centers for Medicare & Medicaid Services (CMS). These standards address preauthorization, balance billing, requests needing documentation, general compliance and fraud/waste/abuse, regulations and guidance, Medicare Advantage marketing by providers, and STAR ratings.
Learn about and access Select Health's online preauthorization tool, CareAffiliate.
Access preauthorization forms.
Providers participating on Select Health Medicare have agreed to accept our established fee schedule rates for services rendered to Medicare members. CMS and Select Health do not allow providers to "balance bill" members for covered services beyond these rates. Providers not participating on the Select Health Medicare network who render services to Medicare beneficiaries agree to accept the Medicare allowed amounts and also to not balance bill beneficiaries.
Please note:
Contrary to original Medicare, CMS does not permit the use of Advance Beneficiary Notices (ABNs), or waiver of liability, for members of any Medicare Advantage plan, such as Select Health Medicare.
As an alternative to issuing an ABN, you can use a “preservice denial” to bill a member for non-covered services instead of an ABN or similar form, which are subject to CMS audit and corrective action. A preservice denial ensures all parties are informed of the noncovered service, makes the member aware of their appeal rights, and supports accurate reporting.
To obtain a preservice denial, be sure to use:
Providers will receive a copy of the denial notice when the preservice is approved or denied.
For more information, access the following CMS resources:
Some services require additional information from the provider before we can review and process the claim appropriately. Our documentation process for a Select Health Medicare request requires that we may:
To expedite original request processing, please include missing documentation with the requesting letter instead of with a new request. This will avoid having your request mistakenly entered as a corrected or duplicate request.
Reporting FWA: Anonymous reporting and interpretation services are available. To report potential fraud, waste, and abuse, call the Compliance Hotline at 800-442-4845.
To speak to someone or ask questions about plan benefits or coverage, call Member Services at 800-538-5038 (TTY: 711). Learn more by accessing the CMS Fraud Prevention Toolkit by calling 800-Medicare (800-633-4227). TTY/TDD users should call 877-486-2048. A Medicare Customer Service representative can answer your questions 24 hours a day, 7 days a week. For additional information, please see the Medicare Compliance Program website.
Regulations governing the MA program are found at 42 CFR Part 422 and Part 423. Review the Code of Federal Regulations (CFR).
CMS provides additional guidance through the CMS Internet-Only Manuals as follows:
CMS requires MA plans and their FDRs to check the OIG List of Excluded Individuals and Entities (LEIE) and GSA System for Award Management (SAM) lists each month for those who have been excluded or precluded from participation in federal programs.
Note that: In addition, the CMS Preclusion List includes providers (individuals and entities) who are currently precluded from receiving payment from the Medicare plan.
Download guidance: Skilled Nursing Facilities (SNFs) & Home Health Providers: Notices of Medicare Non-Coverage Required for Select Health Medicare
Select Health strives to provide the same superior service to patients that they provide to providers. If providers have a patient who has questions or concerns about Medicare Advantage plans, or just general questions, have them call Select Health at 800-538-5038.
For more information about CMS guidelines related to provider-based marketing activities, please review the Dos and Don’ts of Medicare Advantage Plan Marketing document.
Each year, CMS measures the quality and value of certified health plans like Select Health Medicare. Medicare-certified health plans, both Part C (Medicare Advantage) and Part D (Prescription Drug), are rated on a star scale. The scale ranges from one to five stars, with five stars representing the highest quality. Medicare Advantage plans, like Select Health Medicare, with prescription drug coverage contracts are rated on up to 42 unique quality and performance measures. Some examples of the categories include:
CMS Star ratings can help members compare different plans’ quality and performance when they evaluate their current plans each year during the annual election period (October 15 to December 7). This is the best time for members to make sure their plan will meet their healthcare needs for the coming year and make any necessary adjustments.
Ultimately, star ratings result in added benefits like exercise plans, vision, dental, lower premiums, and lower copayments for the members. Any revenue bonus the plan receives for these ratings must be reinvested back to the member.
To determine overall performance ratings, Medicare uses:
The Health Outcomes Survey (HOS) is administered annually by a CMS-approved vendor and is mandatory for MA plans. Each year, a random sample is drawn from the MA plan and selected to participate. The HOS queries Medicare Advantage plan members about their health status and the discussions they have with their providers that occur during a clinic visit or an annual wellness visit. CMS uses the results of this survey to monitor health plan performance and drive quality improvement, and results impact annual CMS Star ratings.
Learn more at the Health Outcomes Survey (HOS) site or call 800-538-5054.