It’s Time to Get Certified for 2026: Product Training Opened July 16th
Annual certification for Select Health Medicare plans is right around the corner. To be ready to sell 2026 plans, you’ll need to complete both your CMS-compliant certification and our Select Health product training. Don’t wait—knock out your training early and be ready to sell day one!
Here’s what you need to know:
Complete AHIP or NABIP First
We accept both AHIP and NABIP certification.
When completing your training, please electronically transmit your results to Select Health so that we can receive your certification automatically—no need to send us a certificate.
Use this link to get started with AHIP: ahipmedicaretraining.com/clients/selecthealth
Product Training Available Now
- Access the training here
- You do not need to log into Link to complete the training
- Be sure to follow all instructions and save your completion certificate
- Product training must be completed by December 31, 2025
Want to access it through Select Health Link?
You can also log into Link and find the training under the Medicare tab > 2026 Medicare Product Training.
Stay Active in Link
To avoid login issues, make sure you’re using Link regularly. Accounts not accessed within the past year may be disabled.
Bookmark after you’ve fully logged in with 2-step verification: Link
Need help?
- For login or verification help, contact the MAAS team at 801-442-7320 or MAAS@selecthealth.org
- For appointment or onboarding questions, contact Stephanie.Crandall@selecthealth.org
- For Link training, contact Clifton.Carling@selecthealth.org
Member Newsletter Now Available: Help Members Make the Most of Their Plan
We recently released the 2025 Summer Select Health Medicare member newsletter, filled with helpful reminders and wellness tips to encourage year-round engagement.
This edition includes a variety of topics to help members get the most out of their plan—like preventive care, care coordination resources, wellness programs, and ways to stay active and connected.
What you should know:
This is a great touchpoint to reinforce your value and support retention. Feel free to ask your clients if they received it and offer to walk through any topics they may have questions about.
You can also view or share the newsletter here.
If you’d like ideas on how to use the newsletter in your member follow-ups or retention strategy, reach out to the MAAS team at 801-442-7320 or MAAS@selecthealth.org—we’re happy to help.
Know Your Member ID Cards: Helping You Understand What Your Clients Will Receive
Select Health Medicare members may receive several different ID cards after enrollment, each tied to specific parts of their plan. You can help reduce confusion and improve member experience by understanding what each card does and how it should be used.
Original Medicare Card
All Medicare beneficiaries receive a red, white, and blue Original Medicare card from the federal government. It includes a unique Medicare Number (different from their Social Security number) and shows whether they have Part A, Part B, or both.
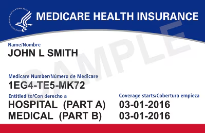
Important for agents to know: Once a member enrolls in a Select Health Medicare plan, they do not need to present their Original Medicare card when receiving care. It may confuse the provider office on what plan to bill or how they determine coverage. Advise them to keep it in a safe place and not share their Medicare Number unless absolutely necessary.
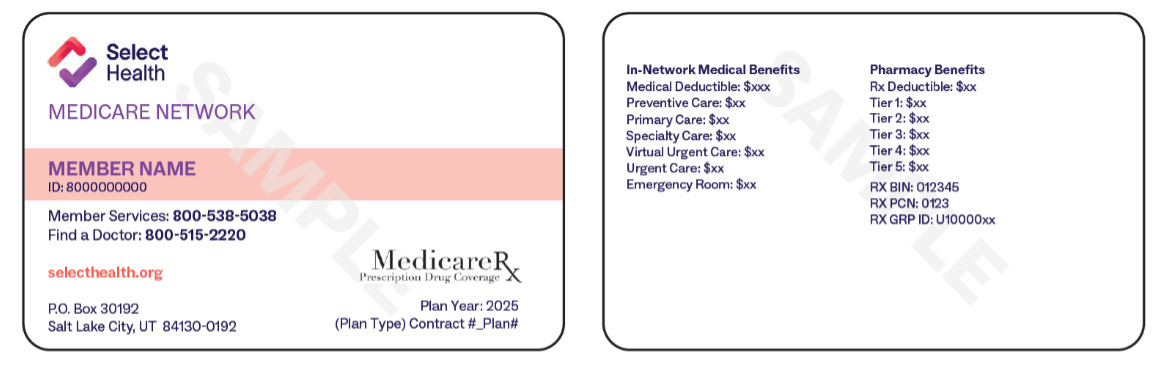
Select Health Medicare ID Card
This is the primary card members should use when seeking care. It is mailed after enrollment and includes:
- The member’s Select Health ID number
- Plan name and key benefit info
- Contact numbers for Member Services
Encourage your clients to present this card at appointments and to carry it with them.
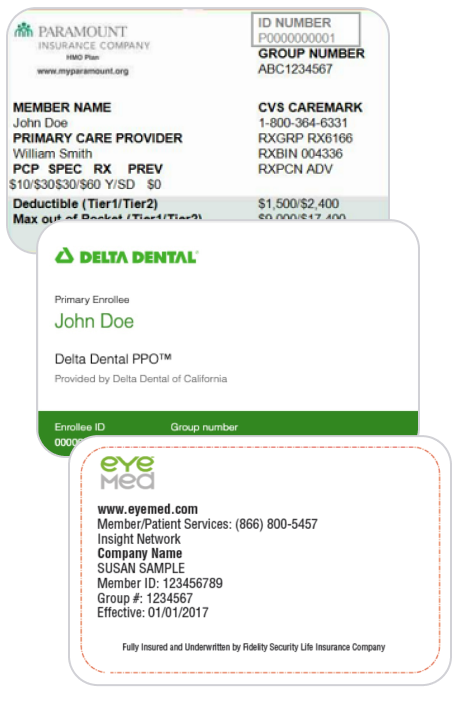
Dental and Vision ID Cards
If the member’s plan includes dental or vision benefits through a third-party provider (such as Delta Dental of Idaho, EyeMed, Paramount Dental, or Select Health Dental), they will receive a separate card for those benefits.
Remind members to watch for these additional cards and bring them when accessing those services.
Flex Card (NationsBenefits Mastercard®)
Members who are eligible for wellness, OTC, utility, or grocery funds will receive a Flex Card after enrollment. This functions like a prepaid debit card and must be activated upon receipt.
Depending on the member's plan, it may be used for:
- OTC, wellness, and Health Living
- Food and Produce
- Utility benefits (DSNP only)
Remind members to register and manage their Flex Card online at selecthealth.nationsbenefits.com.

Lost or Missing Cards? Here’s What to Do
If a member reports a lost or missing card, they can call Member Services at 855-442-9900 (TTY :711) to receive assistance in replacing their Select Health cards. To replace their Original Medicare card, they must contact their local SSA office. The replacement is typically mailed out within 7–10 business days.
You can also request a new card for them by calling the Medicare Advantage Agent Support (MAAS) line at 801-442-7320 or emailing MAAS@selecthealth.org.
Stay Sharp: Ongoing Agent Trainings Available Every Month
Whether you're a new agent or want to brush up before AEP, our monthly agent trainings are a great way to stay informed, confident, and connected.
We offer both in-person and virtual options to fit your schedule:
Utah Agents
- Virtual trainings: 1st and 3rd Thursday of each month
Colorado Agents
- Virtual trainings: 2nd and 4th Thursday of each month
Nevada Agents
- Virtual trainings: 1st and 3rd Wednesday of each month
Our sessions cover:
- Plan benefits and positioning
- Enrollment tools and process tips
- Compliance reminders
- Member engagement strategies
- Live Q&A with our training team
Want to attend?
Reach out to the Agent Training Team or Medicare Advantage Agent Support (MAAS) line at 801-442-7320 or email MAAS@selecthealth.org for schedules and registration info.
Help Members Get a House Calls Visit—and Earn $50
If you're working in Utah or Colorado, there's a simple way to support member health and earn extra this summer. When you help a new Select Health Medicare member complete a House Calls doctor referral form, you’ll receive a $50 incentive for making the connection.
Here’s how it works:
- After enrollment, assist your member with filling out the House Calls referral form in Link.
- Submit the form within 14 days of the member’s effective date.
- Once submitted, you’ll receive $50 for your referral. This incentive is only available to licensed agents writing business in Utah or Colorado.
These in-home visits give members one-on-one time with a licensed clinician, helping improve preventive care and satisfaction, especially for those with chronic or complex conditions.
Questions? Contact your SAE or the Medicare Advantage Agent Support (MAAS) line at 801-442-7320 or email MAAS@selecthealth.org.
Heads-Up: HOS Survey Will Be Mailing Soon—Here’s What to Know
The annual Health Outcomes Survey (HOS) will be mailed soon to a random selection of Select Health Medicare members. You may get questions from your clients about this mailing—here’s what you need to know.
What is the HOS survey?
The Health Outcomes Survey is a CMS-required questionnaire that asks members about their health status, physical and mental well-being, and how their care is supporting their overall health.
It’s different from CAHPS or other satisfaction surveys—HOS focuses on clinical outcomes over time, such as mobility, activity level, fall risk, and emotional health.
Who gets it?
Only a random sample of members receive the survey. If your client didn’t receive it, no action is needed.
Why is it important?
HOS results help CMS and Select Health evaluate how well we’re supporting members’ long-term health. It also affects our Star Ratings, which determine how plans are evaluated and funded.
What can you do?
If one of your clients receives the HOS survey and asks about it, you can reassure them with the following:
- Participation is voluntary, but their responses help improve care for all members
- Answers are confidential and protected
- The survey helps ensure Select Health continues to offer strong, supportive benefits
Need help answering questions?
The Medicare Advantage Agent Service (MAAS) team is always available to support you. Reach out at 801-442-7320 or MAAS@selecthealth.org if you need help responding to member concerns.