We’ll Continue Paying Full and Timely Commissions
At Select Health, we value the important work you do to help clients find the right Medicare Advantage coverage. We also want to be transparent and reassure you that Select Health will continue paying commissions in full and on schedule for all Medicare Advantage plans.
Our agents are key to our success, and we’re committed to supporting you with consistent, reliable payments.
View the 2026 commission schedule here.
If you have questions, please contact your Sales Account Executive or contact our Medicare Advantage Support (MAAS) team at 801-442-7320 or MAAS@selecthealth.org.
Preparing for Member Questions in the New Year
As we wrap up another Annual Enrollment Period (AEP), we want to sincerely thank you for your hard work and dedication. Your efforts make a real difference in helping members feel confident about their Medicare decisions and we appreciate everything you do to support them.
What’s Next for Your Members?
As your new members transition into their plans, they’ll begin receiving a series of onboarding communications to help them understand and use their benefits. Below is a quick overview of what they can expect—and when—so you’re prepared to answer common questions at the start of the year.
Member Guide
Timeline: Typically arrives within 2-3 weeks of the effective date
What it includes: A helpful guide members can use to learn about their supplemental benefits and how to use them.
Evidence of Coverage (EOC)
Timeline: Typically arrive before the effective date or within 7-10 days after enrollment
What it includes: The official plan document outlining covered services, costs, and member rights and responsibilities. Encourage members to keep this document for reference throughout the year.
Member ID Cards (Medical, Dental, and Vision)
Timeline: Typically arrive before the effective date or within 7-10 days after enrollment
What to know: Members may receive multiple cards, including their medical ID card, dental ID card, and Benefits Mastercard® prepaid card (Flex Card).
For more details on different ID cards and when to use them, see the full ID article in this issue.
Flex Card (Benefits Mastercard® Prepaid Card)
Timeline: Usually mailed before the effective date or within 7-10 days after enrollment
Reminder: Renewing members do not receive a new Flex Card every year.
Reminder Members Will Receive
During the first few months of coverage, members will also receive helpful reminders about:
- Using their Flex Card – How to access and use eligible benefits
- Completing the Health Risk Assessment (HRA) – Available online or by paper
- Scheduling their Annual Wellness Visit — Encourage proactive, preventive care
These touchpoints are designed to help members feel supported and get value from their plan early in the year.
If you have any questions, please contact your Sales Account Executive or the Medicare Advantage Support (MAAS) team at 801-442-7320 or MAAS@selecthealth.org.
Know Your Member ID Cards: Helping You Understand What Your Clients Will Receive
Select Health Medicare members may receive several different ID cards after enrollment, each tied to specific parts of their plan. You can help reduce confusion and improve member experience by understanding what each card does and how it should be used.
Original Medicare Card
All Medicare beneficiaries receive a red, white, and blue Original Medicare card from the federal government. It includes a unique Medicare Number (different from their Social Security number) and shows whether they have Part A, Part B, or both.
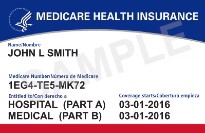
Important for agents to know: Once a member enrolls in a Select Health Medicare plan, they do not need to present their Original Medicare card when receiving care. It may confuse the provider office on what plan to bill or how they determine coverage. Advise them to keep it in a safe place and not share their Medicare Number unless absolutely necessary.
Select Health Medicare ID Card
This is the primary card members should use when seeking care. It is mailed after enrollment and includes:
- The member’s Select Health ID number
- Plan name and key benefit information
- Contact numbers for Member Services
Encourage your clients to present this card at appointments and to carry it with them.
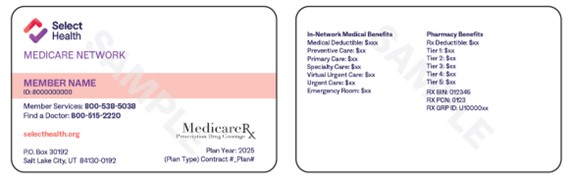
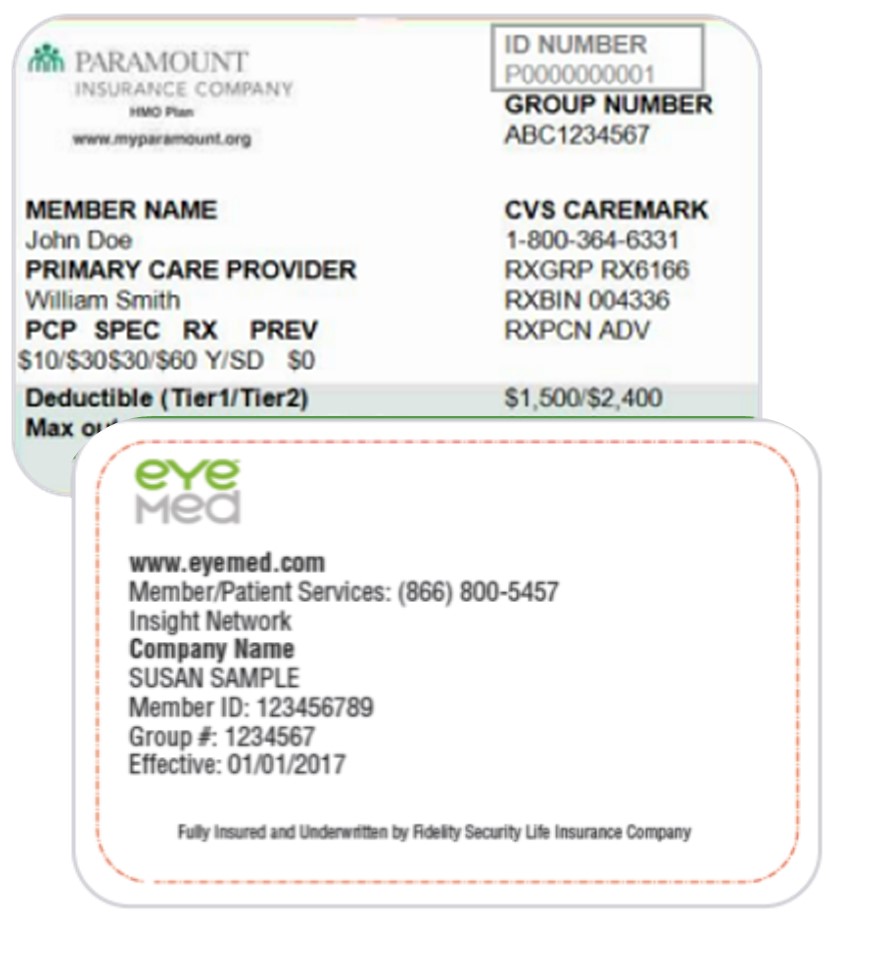
Dental and Vision ID Cards
If the member’s plan includes dental or vision benefits through a third-party provider (such as EyeMed, Paramount Dental, or Select Health Dental), they will receive a separate card for those benefits.
Remind members to watch for these additional cards and bring them when accessing those services.
NationsBenefits Mastercard® Prepaid Card (Flex Card)
Members who are eligible for wellness, OTC, utility, or food and produce funds will receive a Flex Card after enrollment. This functions like a prepaid debit card and must be activated upon receipt. Depending on the member’s plan, it may be used for:
- OTC, wellness, and Healthy Living
- Food and Produce
- Utility Benefits (D-SNP only)
Remind members to register and manage their Flex Card online at selecthealth.nationsbenefits.com.

Lost or Missing Cards?
If a member reports a lost or missing card, they can call Member Services at 855-442-990 (TTY: 711) to receive assistance in replacing their Select Health cards. To replace their Original Medicare card, they must contact their local SSA office. The replacement is typically mailed out within 7-10 business days.
You can also request a new card by contacting the Medicare Advantage Agent Support (MAAS) team at 801-442-7320 or MAAS@selecthealth.org.
Wellth Rewards: Quick Overview for Agents
Wellth Rewards is an optional program for Select Health Medicare members that helps them build healthy habits and earn up to $360 per year. Members earn rewards by completing daily health tasks, like taking medications or tracking health habits. Participation does not affect coverage or benefits.
Important to Know
- Wellth Rewards is separate from the Healthy Living program
- Members will receive a separate rewards card to use for Wellth Rewards incentives.
Who It’s For
The program is available to targeted Select Health Medicare members in Colorado, Nevada, and Utah who meet specific participation criteria.
Members who qualify will receive direct outreach from Wellth inviting them to enroll.
This is not a general enrollment program, and members cannot self-refer without an invitation.
How Members Get Started
Option 1: Check Eligibility by Phone
- Members can call the Wellth support team at 877-553-5118 (TTY: 711) to confirm eligibility. If they qualify, enrollment can be completed over the phone.
Option 2: Download the App
Members who have been invited and confirmed in the system, can download the Wellth Rewards app on their smartphone.
- Complete a quick signup process
- The app will guide them through daily health check-ins
Once Enrolled, Members:
- Receive reminders in the app
- Take a quick photo of their healthy habit (like taking medication)
- Earn monthly rewards that can be used for everyday essentials like groceries, gas, and personal care items
Help Members Navigate the New Silver&Fit Benefit
Many Select Health Medicare plans have transitioned from Wellness Your Way to the Silver&Fit® Healthy Aging and Exercise Program for 2026. Silver&Fit offers a flexible fitness benefit designed to help members stay active and healthy.
What’s Included
Members can choose from:
- A membership at participating fitness centers or select YMCAs
- Access to on-demand workout videos and virtual classes
- Personalized workout plans
- One Home Fitness Kit per year (like beginner strength, yoga, walking, or fitness trackers)
- Optional activity tracking with the Silver&Fit Connected!™ tool to earn fun rewards
How the Transition Works
Silver&Fit will reach out directly to eligible members with invitations and instructions on how to get started.
How Members Get Started
Once they receive their invitation, members can:
- Visit SilverandFit.com to check eligibility, create an account, and select their fitness option
- Use their Silver&Fit card at their chosen fitness location
- Call Silver&Fit Customer Service at 1-877-427-4788 (TTY: 711) for help
Help Members Use Their Healthy Living Rewards
As a reminder, Select Health Medicare members can earn and spend Healthy Living Rewards by completing eligible wellness activities like annual physicals, flu shots, and routine screenings. These rewards are added to their Benefits Mastercard® prepaid card and can be used on fitness equipment, wellness services, home essentials, dining experiences, and more.
Many members forget to complete their activities or spend their rewards before they expire. That’s where you can help!
- Remind your clients to complete their wellness activities early so they have time to use their rewards.
- Encourage them to log in to their Benefits Pro Portal to check their current reward balance.
- Remind members that rewards expire December 31, though any dollars earned late in the year can be spent through March 31 of the following year.
Your reminders go a long way in helping members get the most from their plan while supporting their overall health and satisfaction.
Learn more about Healthy Living Rewards at selecthealth.org/medicare/wellness/healthy-living.
New Digital Enrollment Guides Now Available
We’re excited to announce the release of our new digital enrollment guides. They are designed to make selling easier, faster, and more convenient.
These digital versions give you instant access to the same great content you’re used to in our printed enrollment guides—now optimized for online use. Whether you’re meeting with clients in person or virtually, you can easily share or reference the guide that matches your service area.
Why You’ll Love the Digital Versions
- Instant access – View or share the guide from any device, no waiting for printed copies.
- Always up to date – Digital versions reflect the most current plan information and details
- Easy to share – Send a quick link to clients via email or text during consultations
- Environmentally friendly – Reduce paper waste while keeping all the same helpful details at your fingertips
Use these guides as a go-to resource to walk clients through plan options, benefits, and next steps for enrollment.
Digital Enrollment Guide Links
- Utah – North
- Utah – South Central
- Utah – DSNP
- Nevada – Standard
- Nevada – DSNP
- Colorado – Front Range
- Colorado – Western Slope
If you have questions, please contact your Sales Account Executive or contact our Medicare Advantage Agent Support (MAAS) team at 801-442-7320 or MAAS@selecthealth.org.